63% of uninsured Nebraska kids are low-income and likely
eligible for Medicaid/CHIP.1
88.6% of Nebraska children are in very good or excellent health.2
2. 2016 National Survey of Children’s Health.
Why does it matter?
All children deserve access to affordable, quality physical and behavioral health care.
Quality and consistent preventive health care, beginning even before birth, gives children the best chance to grow up to be healthy and productive adults.
Adequate levels of immunization, public health efforts to prevent disease and disability, and support for maternal health and positive birth outcomes are examples of measures that help children now and later. Good health, both physical and behavioral, is an essential element of a productive and fulfilling life.
Births
26,594 babies were born in 2016.
Births by race & ethnicity (2016)
- White (77.2%)
- Other/Unknown Race (9.9%)
- Black/African American (7.3%)
- Asian/Pacific Islander (3.8%)
- American Indian/Alaska Native (1.7%)
- Unknown (0.2%)
- Not Hispanic (83.8%)
- Hispanic (16.1%)
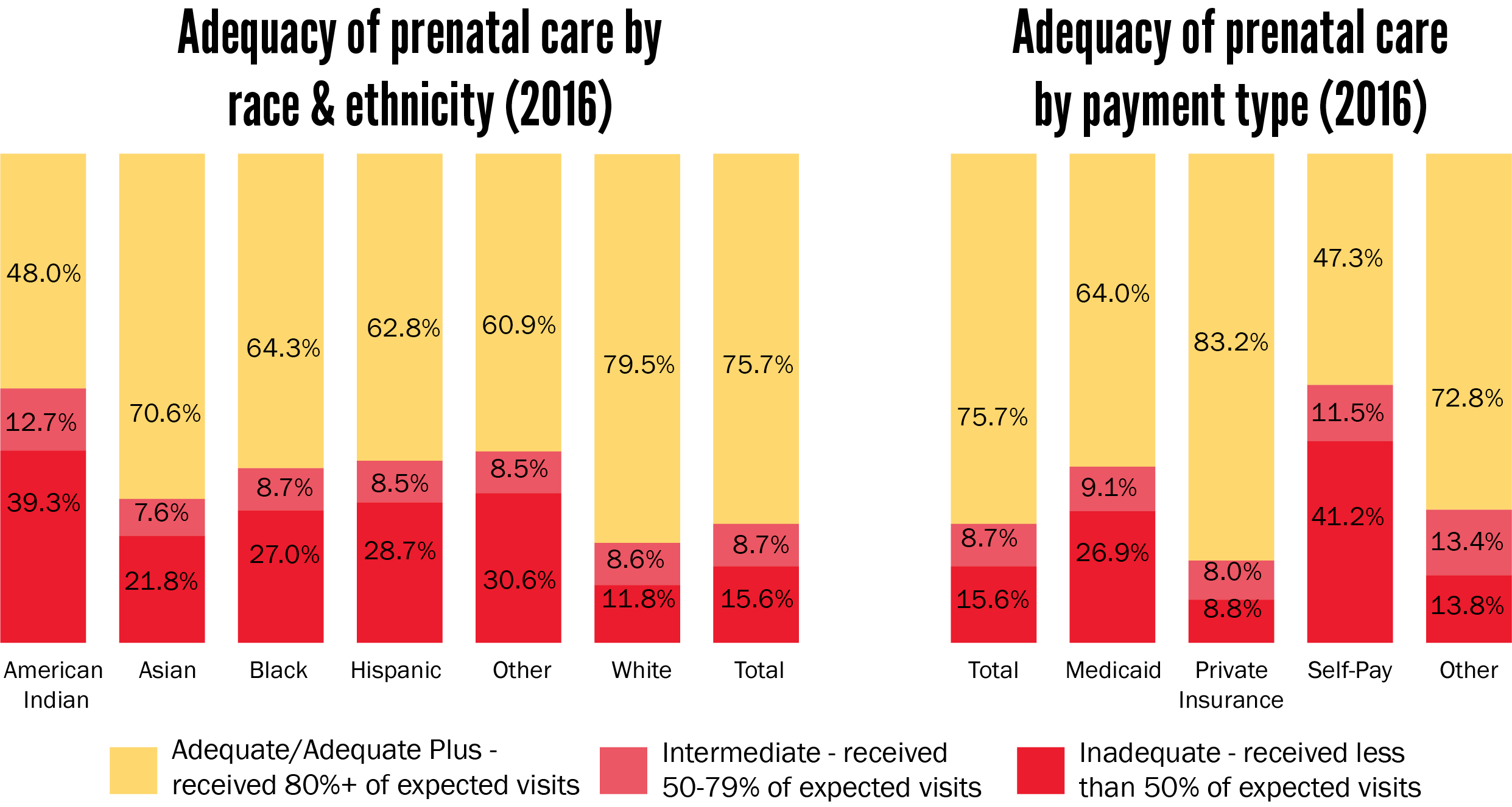
15.6% of babies received inadequate prenatal care.
Women who see a health care provider regularly during pregnancy have healthier babies and are less likely to deliver prematurely or to have other serious pregnancy-related problems. The ideal time for a woman to seek out prenatal care is during her first trimester or even prior to getting pregnant.
Barriers to care can include a lack of any of the following:
• insurance,
• transportation,
• knowledge of where to find care,
• quality treatment at care center,
• translation services, and
• knowledge of importance of care.
Trimester prenatal care began (2016)
- First (73.8%)
- Second (20.2%)
- Third (4.5%)
- None (1.5%)
- First (73.8%)
- Second (20.2%)
- Third (4.5%)
- None (1.5%)
Pre/post-natal health
Folic acid use prior to pregnancy (2015)1
- 4 or more times/week before pregnancy (43.6%)
- 3 or fewer times/week before pregnancy (56.4%)
- 4 or more times/week before pregnancy (43.6%)
- 3 or fewer times/week before pregnancy (56.4%)
Mother’s BMI prior to pregnancy (2015)1
- Underweight before pregnancy (9.2%)
- Normal weight before pregnancy (48.4%)
- Overweight before pregnancy (13.2%)
- Obese before pregnancy (29.2%)
- Underweight before pregnancy (9.2%)
- Normal weight before pregnancy (48.4%)
- Overweight before pregnancy (13.2%)
- Obese before pregnancy (29.2%)
Tobacco use (2016)2
- Did not use tobacco during most recent pregnancy (86.2%)
- Used tobacco during most recent pregnancy (9.9%)
- Smoked in the three months prior to pregnancy
- Did not use tobacco during most recent pregnancy (86.2%)
- Used tobacco during most recent pregnancy (9.9%)
- Smoked in the three months prior to pregnancy
Pregnancy intendedness (2015)*1
- Unintended pregnancy (41.8%)
- Intended Pregnancy (58.2%)
- Unintended pregnancy (41.8%)
- Intended Pregnancy (58.2%)
Breastfeeding (2015)1
- One
- One
Low birth weight (2016)2
- Not low birth weight (93.0%)
- Moderately low birth weight (5.8%)
- Very low birth weight (1.2%)
- Not low birth weight (93.0%)
- Moderately low birth weight (5.8%)
- Very low birth weight (1.2%)
| Domestic violence1 | 2015 |
| Experienced physical abuse from husband or partner in the 12 months before pregnancy | 2.4% |
| Experienced physical abuse by someone other than husband or partner in the 12 months before pregnancy | 2.0% |
| Child birth classes1 | 2015 |
| Participated in child birth classes during most recent pregnancy | 21% |
| Maternal depression1 | 2015 |
| New mothers who experienced maternal depression related to most recent pregnancy | 12% |
1. PRAMS, 2015.
2. Vital Statistics, Department of Health and Human Services (DHHS).
Teen births & sexual behavior
Teen parenting
While teen pregnancy occurs at all socio-economic levels, teen moms are more likely to come from economically-disadvantaged families or to be coping with substance abuse and behavioral problems. Teen birth is highly correlated with child poverty.
In turn, children born to teenage parents are more likely to live in poverty, experience health problems, suffer from maltreatment, struggle in school, run away from home, and serve time in prison. Children of teen parents are also more likely to become teen parents themselves, thus perpetuating the cycle of teen pregnancy and generational poverty.
Teen births are at the lowest point in a decade. In 2016 there were 1,227 babies born to teen mothers, 332 to mother’s who were 10-17 years old, 895 to mother’s who were 18 or 19.2
Teen births (2007-2016)
- Ages 10-17
- Ages 18-19
- Ages 10-17
- Ages 18-19
Teen births by age (2016)
- Ages 18-19 (72.9%)
- Ages 16-17 (22.3%)
- Ages 14-15 (4.5%)
- Ages 10-13 (0.2%)
- Ages 18-19 (72.9%)
- Ages 16-17 (22.3%)
- Ages 14-15 (4.5%)
- Ages 10-13 (0.2%)
Teen sexual behavior1 |
2015 |
|---|---|
| Ever had sexual intercourse | 32.5% |
| Reported having sexual intercourse before age 13 | 3.3% |
| Had sex with four or more people | 8.0% |
| Had sex in the past 3 months | 24.9% |
| Drank alcohol or used drugs before last sexual intercourse | 17.9% |
| Did not use a condom during last sexual intercourse | 43.0% |
| Did not use any method to prevent pregnancy during last sexual intercourse | 17.8% |
HIV/AIDS3
In 2016, there were 12 children ages 0-11 and 14 children ages 12-19 living with HIV.
Since 2007, no children with a diagnosis of HIV or AIDS have died from the disease.
2. Vital Statistics, Department of Health and Human Services (DHHS).
3. HIV Surveillance, Nebraska Department of Health and Human Services (DHHS).
Sexually transmitted infections (STIs) (2007-2016)2
There were 2,554 cases of sexually transmitted infections reported in children ages 19 and under in Nebraska in 2016.
Infant & child deaths
Infant mortality
Infant mortality increased to 6.2 per 1,000 births in 2016 from 5.8 per 1,000 births in 2015.
| Causes of infant deaths (2016) | Number | Percent |
| Maternal and Perinatal | 37 | 22.3% |
| Birth Defects | 31 | 18.7% |
| SIDS/SUDI | 25 | 15.1% |
| Respiratory and Heart | 25 | 15.1% |
| Prematurity | 15 | 9.0% |
| Infection | 8 | 4.8% |
| Accident | 6 | 3.6% |
| Other | 19 | 11.4% |
| Total | 166 |
Child deaths
In 2016, 115 children and youth ages 1 to 19 died of various causes, the most common of which were accidents and suicide.
| Causes of child deaths (2016) | Number | Percent |
| Accidents | 41 | 35.7% |
| Suicide | 20 | 17.4% |
| Cancer | 9 | 7.8% |
| Birth Defects | 7 | 6.1% |
| Homicide | 6 | 5.2% |
| Other | 32 | 27.8% |
| Total | 115 |
Rate of infant mortality per 1,000 births by race and ethnicity (2016)
Child deaths, ages 1-19 (2007-2016)
Health Insurance
Health coverage for Nebraska’s children, ages 17 & under (2016)1
- Public Insurance
- Employer-Based Insurance
- Direct-Purchase Insurance
- Uninsured
- Public Insurance
- Employer-Based Insurance
- Direct-Purchase Insurance
- Uninsured
Access to health care
In 2016, there were 23,514 (5.1%) uninsured children in Nebraska. Of those, 14,856 (66%) were low-income (below 200% of the federal poverty level) and likely eligible, yet unenrolled, in the Children’s Health Insurance Program (CHIP).1
| Percent uninsured children by race/ethnicity (2010-2014)2 | |
| Black/African American | 4.1% |
| Asian or Pacific Islander | 6.0% |
| Other, or 2+ races | 9.4% |
| White, non-Hispanic | 4.2% |
| Hispanic | 11.6% |
| American Indian and Alaska Native | 16.3% |
5.1% of kids did not have health insurance in 2016.1
Medicaid and CHIP served a monthly average of 161,530 children in SFY 2016.3
74.7% of those eligible for Medicaid/CHIP are children, but children only make up 27% of Medicaid costs.3
Nebraska Medicaid average monthly eligible persons by age (SFY 2016)3
- Blind/Disabled (14.7%)
- Aged (8.3%)
- Adults (2.3%)
- Children (74.7%)
- Blind/Disabled (14.7%)
- Aged (8.3%)
- Adults (2.3%)
- Children (74.7%)
Nebraska Medicaid expenditures by age (SFY 2016)3
- Blind/Disabled (45.2%)
- Aged (20.6%)
- Adults (7.2%)
- Children (27.0%)
- Blind/Disabled (45.2%)
- Aged (20.6%)
- Adults (7.2%)
- Children (27.0%)
CHIP/Medicaid enrollment (SFY 2016)3
- Medicaid (81.6%)
- CHIP (18.4%)
- Medicaid (81.6%)
- CHIP (18.4%)
2. U.S. Census Bureau, 2015 American Community Survey 5-year estimates, Tables C27001B-I.
3. Financial and Program Analysis Unit, Nebraska Department of Health and Human Services (DHHS).
Notes: “Children” category combines Medicaid and CHIP coverage. “Adults” are those aged 19-64 receiving Aid to Dependent Children, or temporary cash assistance through the state of Nebraska.
Behavioral Health
Estimating mental health needs
Many children in Nebraska deal with behavioral health problems that may affect their ability to participate in normal childhood activities.
The National Survey of Children’s Health estimated the number of Nebraska children facing the following disorders:
- Anxiety: 16,462
- ADD/ADHD: 22,444
- Mental or Behavioral Health Condition needing treatment: 39,080
- Depression: 13,600
- Autism Spectrum Disorder: 7,575
| Considered suicide in last 12 months (2015)3 | |
| Seriously considered suicide | 14.6% |
| Had suicide plan | 13.3% |
| Made suicide attempt | 8.9% |
Children receiving community-based mental health services (2016)1
- Mental Health
- Substance Abuse
- Mental Health and Substance Abuse
- Mental Health
- Substance Abuse
- Mental Health and Substance Abuse
2. Financial and Program Analysis Unit, Department of Health and Human Services (DHHS).
3. 2011/12 National Survey of Children’s Health.
4. 2016 National Survey of Children’s Health.
23,937 Nebraska children received mental health and substance abuse services through Medicaid or CHIP in FY 2016.2
20.6% of children four months to five years were at moderate to high risk of behavioral or developmental problems based on parents’ specific concerns.3
72.9% of children needing mental health counseling actually received it.4
24.1% of teens felt sad or hopeless (everyday for 2+ weeks so that activity was stopped in last 12 months).5
Regional centers (2016)1
102 males
received services at Hastings Regional Center, a chemical dependency program for youth from the Youth Rehabilitation & Treatment Center (YRTC) in Kearney.
49 males
received services from Lincoln Regional Center at the Whitehall Campus.
Health Risks
| Motor vehicle behavior among high schoolers | 2015 |
| Rarely or never wore a seat belt | 11.3% |
| In past 30 days, rode in a vehicle driven by someone who had been drinking alcohol | 22.3% |
| In past 30 days, drove a motor vehicle after drinking alcohol | 10.1% |
| In past 30 days, texted or emailed while driving a car or other vehicle | 49.4% |
| Injuries and violence among high schoolers | 2015 |
| In past 12 months, was physically hurt on purpose by someone they were dating | 8.1% |
| In the past 12 months, was threatened or injured with a weapon on school property | 7.1% |
| In past 12 months, was bullied on school property | 26.3% |
| Has ever been physically forced to have sexual intercourse | 8.3% |
| In past 12 months, was in a physical fight | 2.8% |
| In past 12 months, was electronically bullied | 18.9% |
| Alcohol and other drugs among high schoolers | 2015 |
| Ever used marijuana | 26.6% |
| Ever used any form of cocaine | 5.3% |
| Ever used meth | 4.2% |
| Ever used ecstasy or MDMA | 5.1% |
| In past 12 months, offered, sold, or given an illegal drug by someone on school property | 19.9% |
| Ever tried smoking | 31.4% |
| Currently uses smokeless tobacco | 9.3% |
| In past 30 days, had at least 1 drink of alcohol | 22.7% |
| In past 30 days, had 5 or more drinks in a row within a couple of hours | 14.3% |
| Ever took prescription drugs without a doctor’s prescription | 13.5% |
| Currently smokes | 13.3% |
Motor vehicle accidents (2016)
18 children died and 177 children suffered disabling injuries in motor vehicle accidents.
- 51 were not using a seatbelt
- Alcohol was involved in 23
Blood Lead Level Testing (2016)
Exposure to lead may harm a child’s brain and central nervous system. Even low blood lead concentrations can cause irreversible damage such as:
- impaired physical and cognitive development,
- delayed development,
- behavioral problems,
- hearing loss, and
- malnutrition.
The Statewide Blood Lead Testing Plan has detailed guidance on recommendations for when children should have their blood tested for lead. The Centers for Disease Control uses a reference level of 5 micrograms per deciliter to identify children as having an elevated blood lead level.
In 2016:
34,813 children were tested.
411 had elevated blood
lead levels,
representing 1.2% of
all children tested.
Obesity, dieting, activity, and eating habits
| In past 7 days did not eat fruit or drink 100% fruit juice | 5.6% |
| In past 7 days did not eat vegetables | 6.4% |
| Were currently overweight or obese according to CDC growth charts | 29.9% |
| In past 7 days did not participate in at least 60 minutes of physical activity on any day | 14.1% |
Adverse Childhood Experiences
Adverse childhood experiences (ACEs) are potentially traumatic events that can have negative, lasting effects on health and well-being.
Number of ACEs (2016)
- 0 ACEs (58%)
- 1-2 ACEs (22%)
- 3+ ACEs (20%)
- 0 ACEs (58%)
- 1-2 ACEs (22%)
- 3+ ACEs (20%)
Percent of children by ACE
Domestic violence & sexual assault*
Nebraska’s Network of Domestic Violence/Sexual Assault Programs includes 20 community-based programs. There are also five tribal programs which comprise the Nebraska Tribal Coalition Ending Family Violence.
Service Participants (2016)*
- Children
- Women
- Men
- Indisclosed
- Children
- Women
- Men
- Indisclosed
Source: Nebraska Coalition to End Sexual and Domestic Violence.
Services provided to children served (2016)*
Health Services
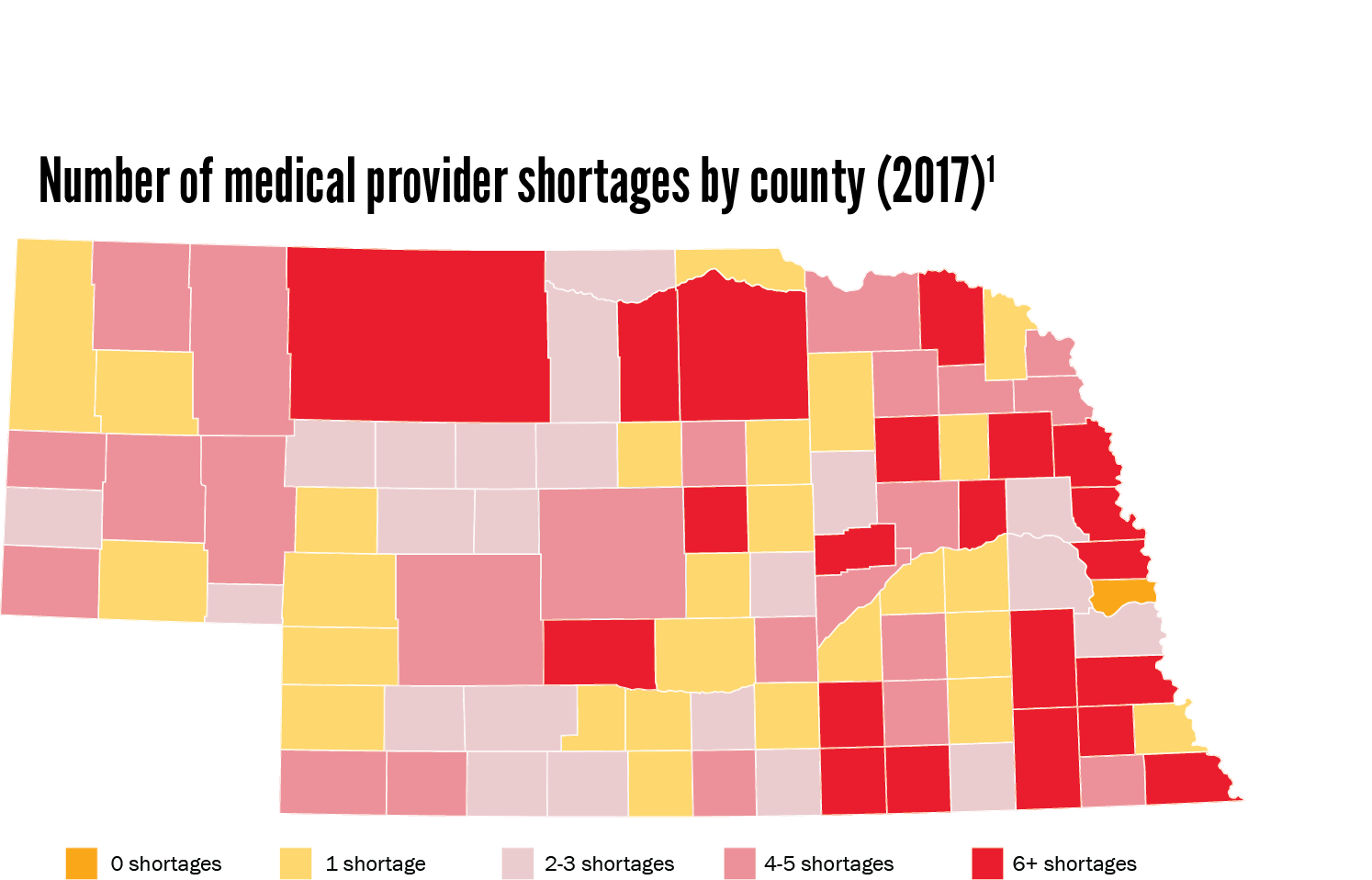
Medical provider shortage
Health professional shortage areas are designated as having too few primary medical, dental, or mental health care providers.
Immunizations (2016)3
80.6% of Nebraska children had received the primary immunization series* by age three.
80.2% of Nebraska teens were immunized against meningitis caused by types A, C, W, and Y.
50.6% of Nebraska teen girls and 41.3% of Nebraska teen boys completed their HPV vaccine series.
79.2% of children had a preventive medical visit in the past year.2
81.3% of children had a preventive dental visit in the past year.2
Percent of children with current health conditions (2016)2
- One
- One
Medical home (2016)2
A patient-centered medical home is a primary care physician or provider that serves as a child’s usual source of care. It is an important mechanism for coordination of all segments of health – physical, behavioral, and oral.
- 45% do not have a medical home
- 55% have a medical home
2. 2016 National Survey of Children’s Health.
3. Immunization Program, Nebraska Department of Health and Human Services (DHHS).
*Series 4:3:1:3:3:1:4