Every child and family deserves access to affordable, quality physical and behavioral health care.
Quality and consistent preventive health care, beginning even before birth, gives children the best chance to grow up to be healthy and productive adults.
Children and families must be able to access and maintain affordable health insurance, and policies should maximize availability and robust investment in Medicaid and the Children’s Health Insurance Program. Our health care systems and policies should prioritize preventive services including immunization, developmental screenings, early intervention, and home visiting. Policies should promote timely and equitable access to a complete range of health care services within a health home and community-based environments for children and families across the lifespan.
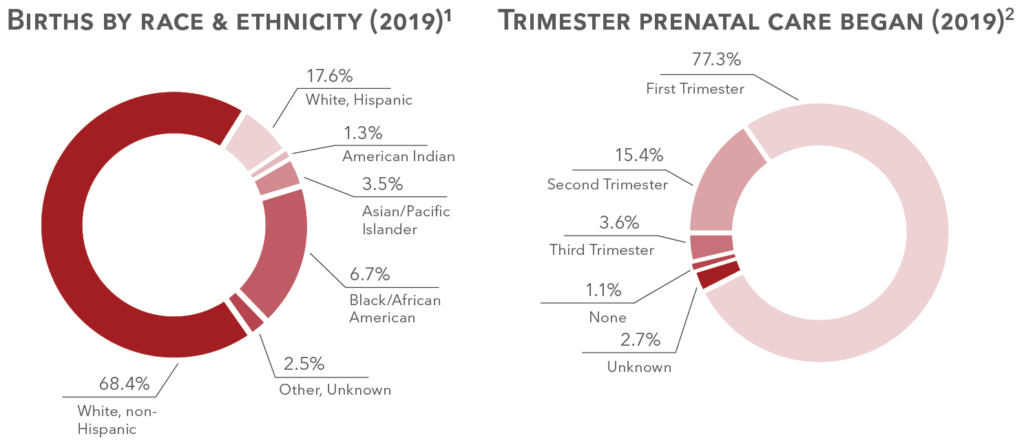
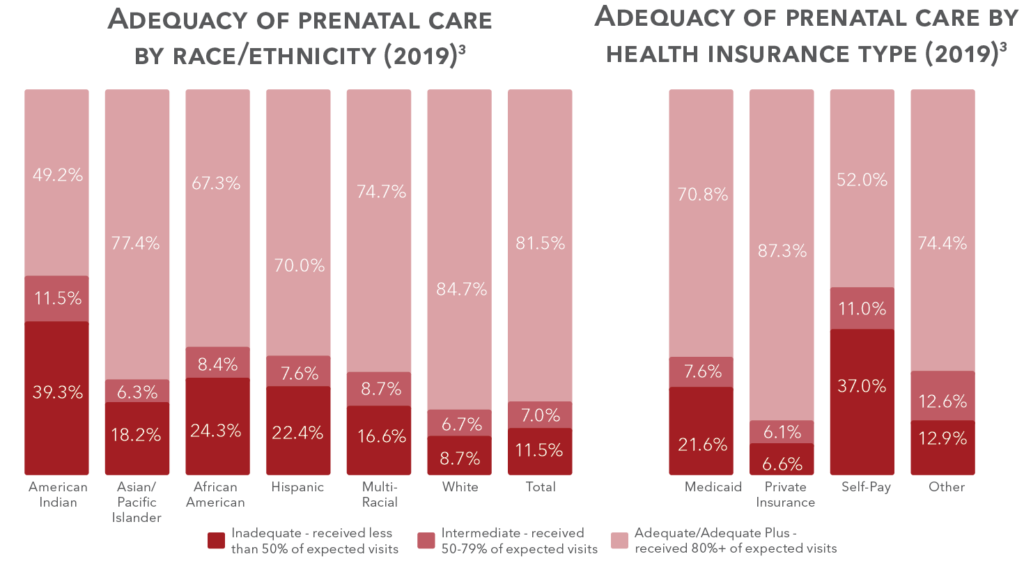
Births
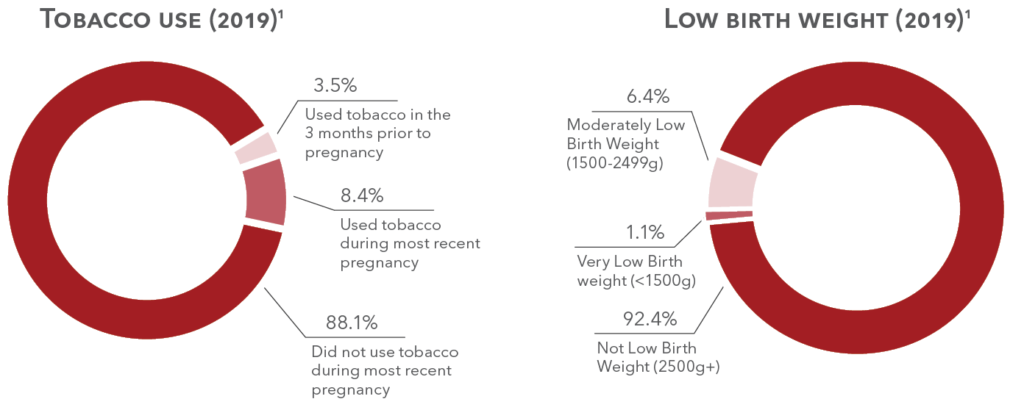
24,758 babies were born in 2019.1
Pre/post-natal health
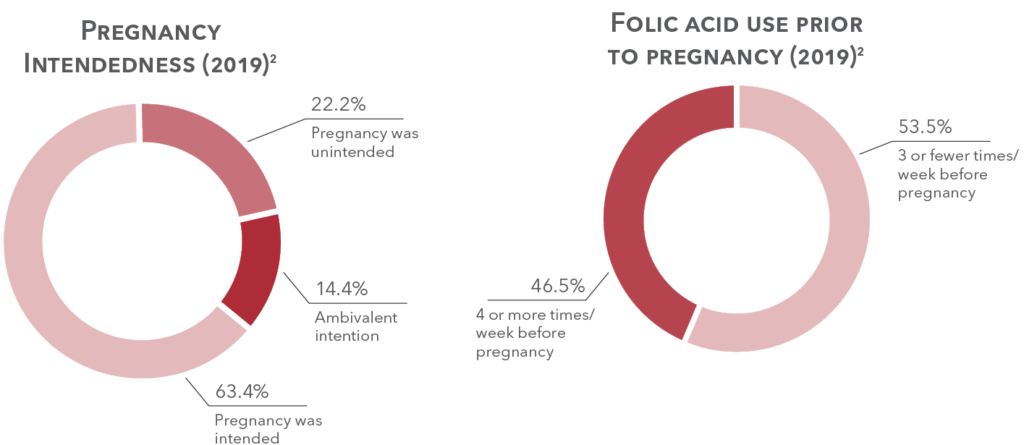
12.3% of new mothers experienced postpartum depression symptoms related to their most recent pregnancy.2
3.6% of women had a home visitor during pregnancy to help prepare for the new baby.2
National Center for Health Statistics (NCHS), Division of Vital Statistics (DVS), Natality on CDC WONDER Online Database,
for years 2016-2019 available October 2020.”
2. PRAMS, 2019.
Teen births & sexual behavior
Teen Births
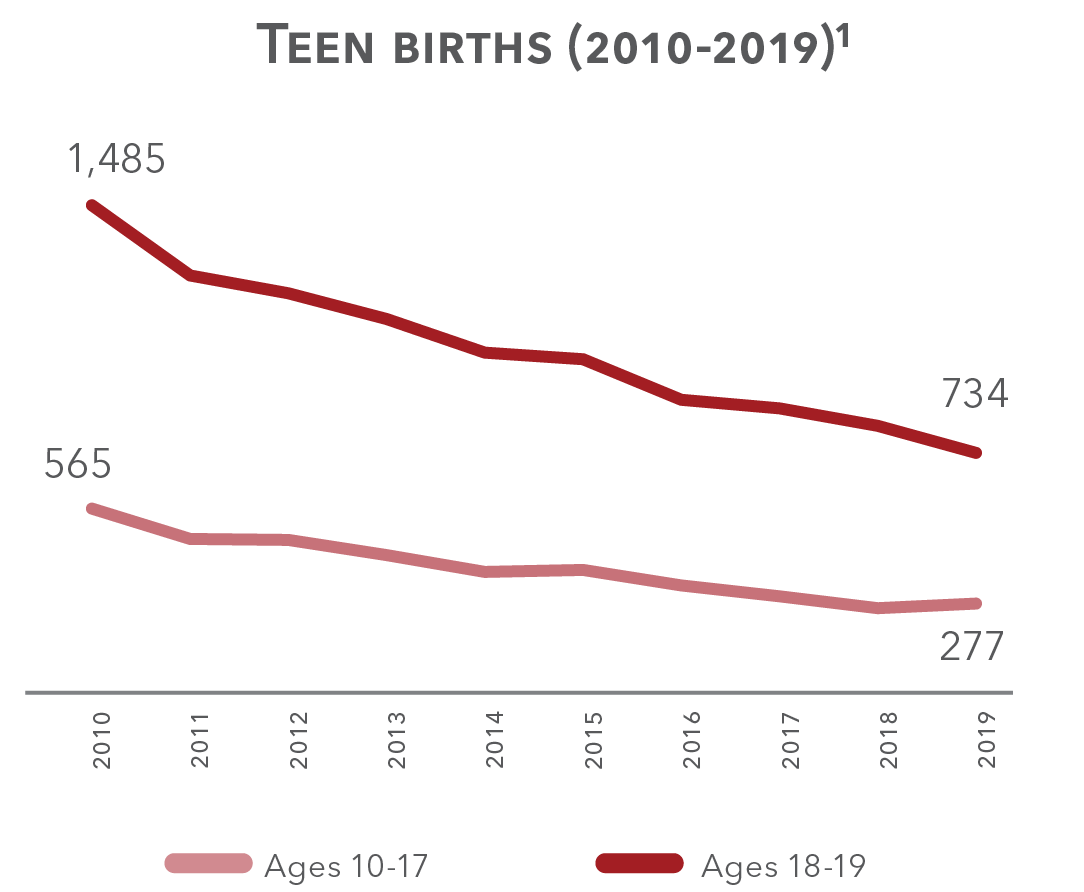
Teen births are at the lowest point in a decade. In 2019 there were 1,011 babies born to teen mothers, 277 to mothers who were 10-17 years old, 734 to mothers who were 18 or 19.¹
Teen births by age (2019)
- Ages 18-19 (72.6%)
- Ages 16-17 (22.7%)
- Ages 14-15 (4.7%)
- Ages 18-19 (72.6%)
- Ages 16-17 (22.7%)
- Ages 14-15 (4.7%)
HIV/AIDS3
In 2019, there were 8 children ages 0-11 and 13 children ages 12-19 living with HIV.
Since 2008, no children with a diagnosis of HIV or AIDS have died from the disease.
2. Vital Statistics, Department of Health and Human Services (DHHS).
3. HIV Surveillance, Nebraska Department of Health and Human Services (DHHS).
Sources:
1. “United States Department of Health and Human Services (US DHHS),
Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Division of Vital Statistics (DVS),Natality on CDC WONDER Online Database, for years 2016-2019 available October 2020.”, Kids Count 2019.
2. Center for Disease Control and Prevention, Youth Risk Behavior Survey, 2019.
3. HIV Surveillance, Nebraska Department of Health and Human Services.
4. STD Prevention Program, Department of Health and Human Services (DHHS).
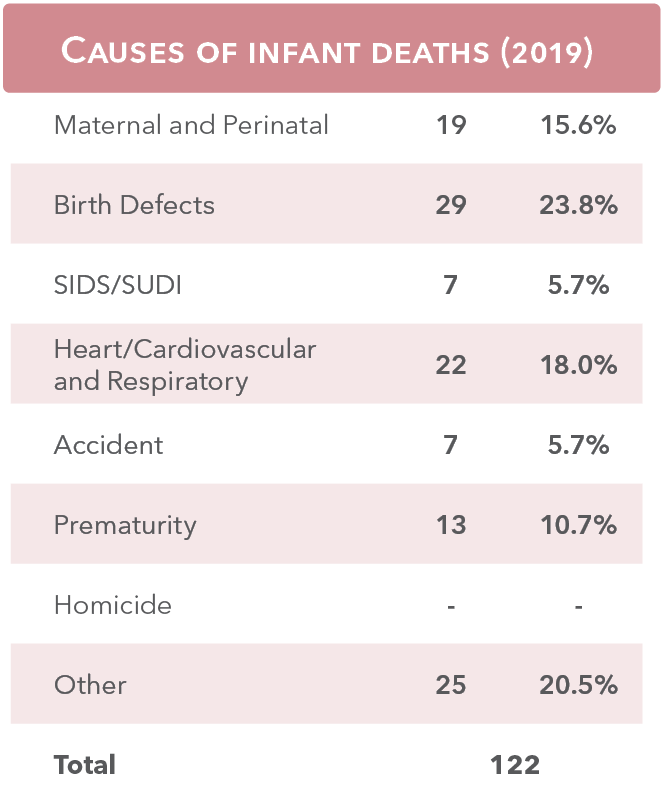
Infant & child deaths
Infant mortality
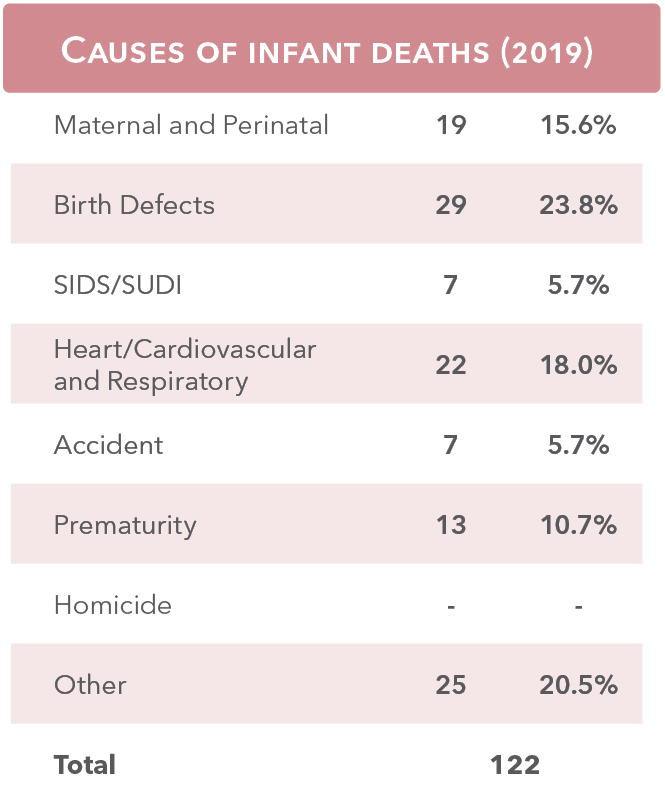
Infant mortality decreased to 4.9 per 1,000 births in 2019 from 5.9 per 1,000 births in 2018.
Pregnancy deaths
8 women died in 2018 due to a cause related to or aggravated by pregnancy or its management.
Rate of infant mortality per 1,000 births by race and ethnicity (2018)
Child deaths, ages 1-19 (2010-2019)
Health Insurance
Health coverage for Nebraska’s children, ages 17 & under (2019)1
- Any
- Public Insurance
- Employer-Based Insurance
- Direct-Purchase Insurance
- Uninsured
- Any
- Public Insurance
- Employer-Based Insurance
- Direct-Purchase Insurance
- Uninsured
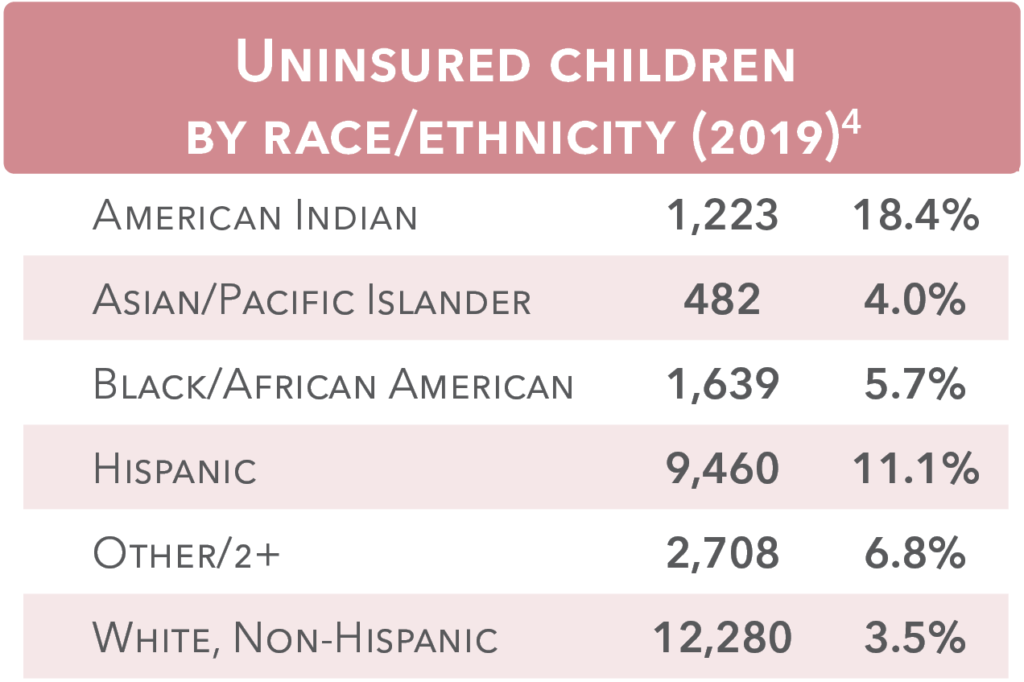
Access to health care
In 2019, there were 26,907 (5.6%) uninsured children in Nebraska. Of those, 15,312 (56.9%) were low-income (below 200% of the federal poverty level) and likely eligible, yet unenrolled in the Children’s Health Insurance Program (CHIP).1
Medicaid and CHIP served a monthly average of 162,207 children in SFY 2019.2
66.9% of those eligible for Medicaid/CHIP are children, but children only make up 27% of Medicaid costs.2
Nebraska Medicaid average monthly eligible persons by age (SFY 2019)2*
- Blind/Disabled (14.6%)
- Aged (7.9%)
- Adults (10.6%)
- Children (66.9%)
- Blind/Disabled (14.6%)
- Aged (7.9%)
- Adults (10.6%)
- Children (66.9%)
Nebraska Medicaid expenditures by age (SFY 2018)2*
- Blind/Disabled
- Aged
- Adults
- Children
- Blind/Disabled
- Aged
- Adults
- Children
CHIP/Medicaid enrollment (SFY 2018)3
- Medicaid (79.2%)
- CHIP (20.8%)
- Medicaid (79.2%)
- CHIP (20.8%)
2. Nebraska Medicaid Annual Report for State Fiscal Year 2019.
3. State Medicaid and CHIP Applications, Eligibility Determinations, and Enrollment Data.
4. U.S. Census Bureau, 2019 American Community Survey 5-year estimates, Table B27001F-G.
* “Children” category combines Medicaid and CHIP coverage. “Adults” are those aged 19-64 receiving Aid to Dependent Children, or temporary cash assistance through the state of Nebraska.
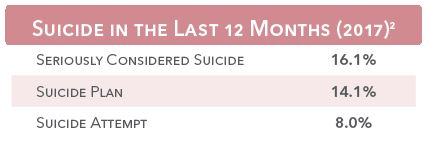
Behavioral Health
An estimated 47,691 Nebraska children have been diagnosed with a mental/behavioral condition needing treatment.1
Many children in Nebraska deal with behavioral health problems that may affect their ability to participate in normal childhood activities. The National Survey of Children’s Health estimates the number of Nebraska children facing the following disorders:¹
• Anxiety: 34,079
• ADD/ADHD: 26,562
• Depression: 17,082
• Autism Spectrum Disorder: 9,753
61.6% of children needing mental health counseling actually received it.¹

Regional centers (2019)3
152 Youths
received services at Hastings Regional Center, a chemical dependency program for youth from the Youth Rehabilitation & Treatment Center (YRTC) in Kearney.
149 youths
received services from Lincoln Regional Center at the Whitehall Campus.
84% of children six months to five years met all four measures of flourishing.¹
• Bounces back quickly when things don’t go their way
• Are affectionate and tender with their parent(s)
• Show interest and curiosity in learning new things
• Smile and laugh a lot
2. Center for Disease Control and Prevention, Youth Risk Behavior Survey, 2019.
3. Division of Behavioral Health, Department of Health and Human Services.
4. Financial and Program Analysis Unit, Nebraska Department of Health and Human Services.
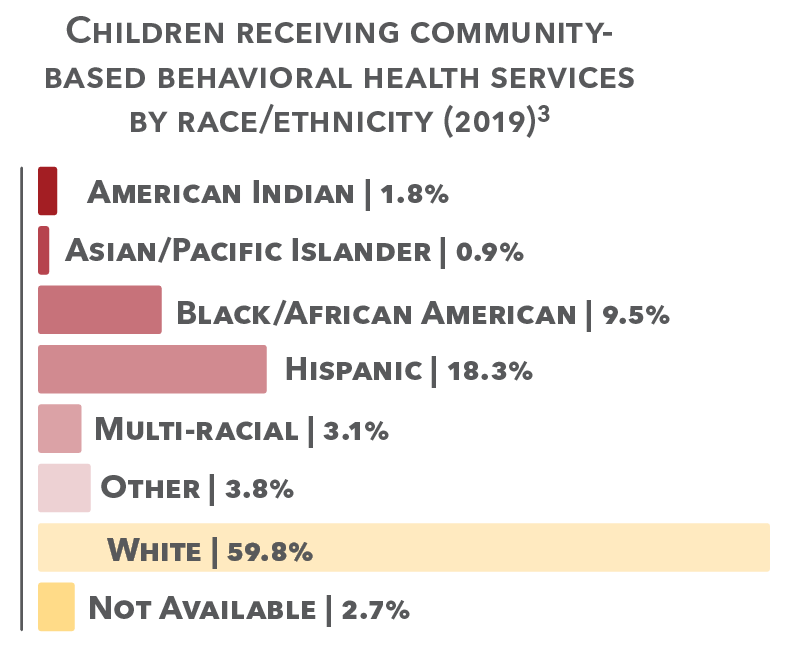
37,887 children received behavioral health services through Medicaid/CHIP from 1,376 providers (FY 2019).³
216 children received developmental services through Medicaid/CHIP (FY 2019).³
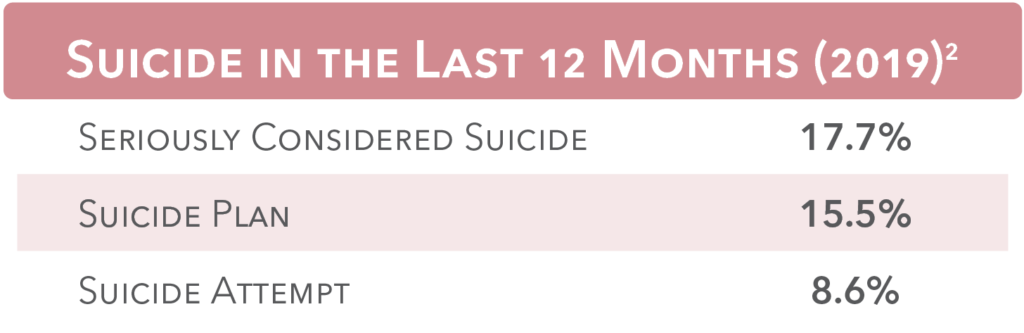
32.0% of teens felt sad or hopeless (everyday for 2+ weeks so that activity was stopped in last 12 months).²
Health Risks
7.4% of high schoolers rarely or never wore a seat belt.1
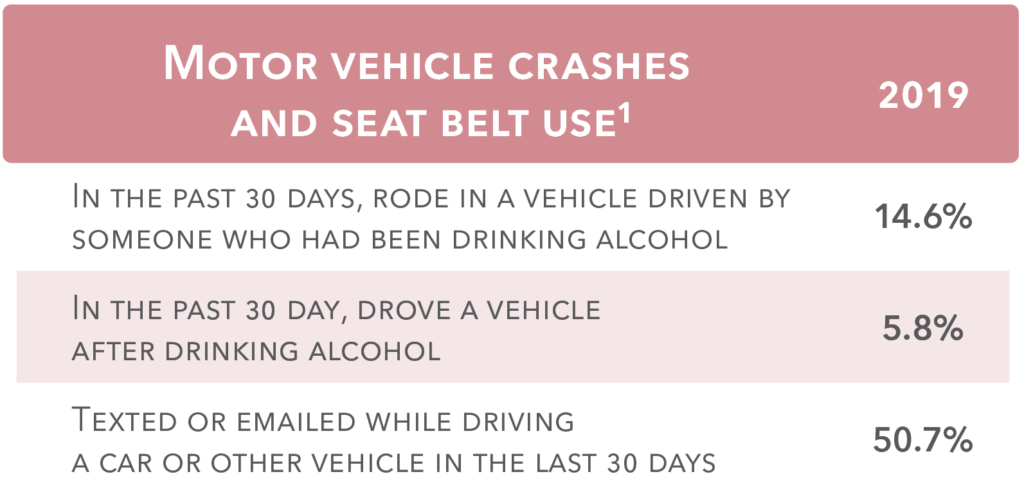
Motor vehicle accidents (2019)2
24 children died and 121children suffered disabling injuries in motor vehicle accidents.
- 25% children who died were not wearing a seatbelt, 28% of those with disabling injuries were not wearing a seatbelt.
- Alcohol was involved in crashes resulting in 1 deaths and 10 disabling injuries.
Blood Lead Level Testing (2019)3
Exposure to lead may harm a child’s brain and central nervous system. Even low blood lead concentrations can
cause irreversible damage such as:
• impaired physical and cognitive development,
• delayed development,
• behavioral problems,
• hearing loss, and
• malnutrition.
In 2019:
39,194 children were tested.
371 had elevated
blood lead levels,
representing 0.9% of
all children tested.
14 Nebraska children ages 1-18 were injured by a firearm necessitating hospitalization in 2019.4
5 were due to
accidental discharge.
7 were due to assault.
1 was undetermined.
1 intentional self-harm.
2. Nebraska Department of Transportation.
3. Nebraska Department of Health and Human Services, Childhood Lead Poisoning Prevention Program.
4. Nebraska Hosptial Information System.
Health Risks
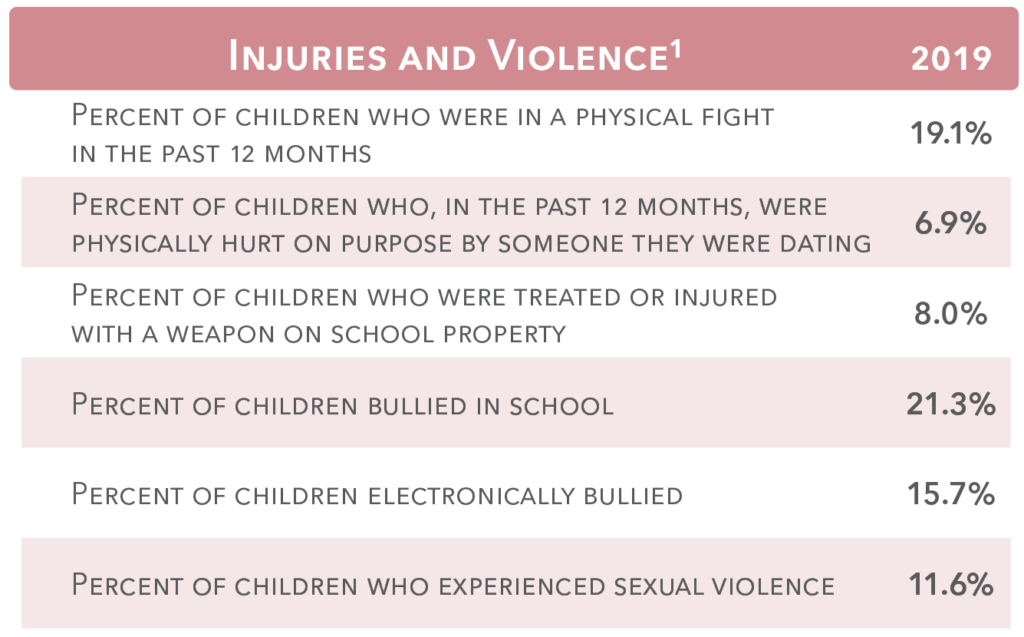
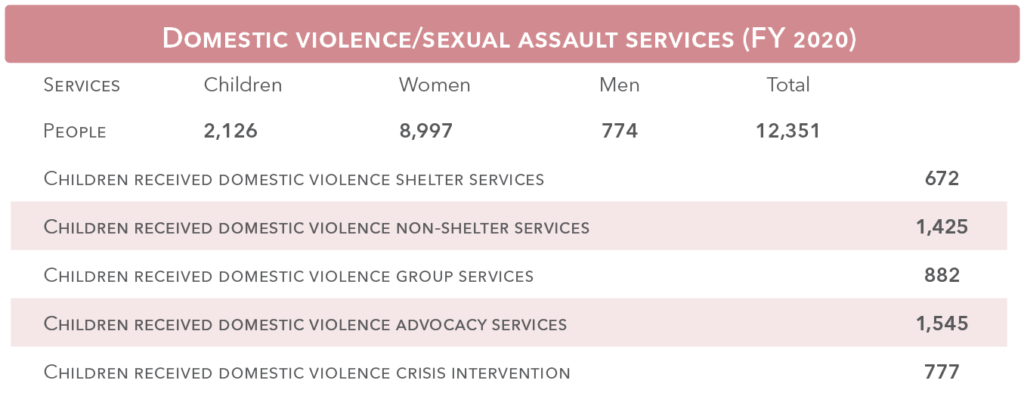
Domestic violence & sexual assault2
Nebraska’s Network of Domestic Violence/Sexual Assault Programs includes 20 community-based programs. There are also four tribal programs which comprise the Nebraska Tribal Coalition Ending Family Violence.
2. Nebraska Coalition to End Sexual and Domestic Violence.
Health Risks
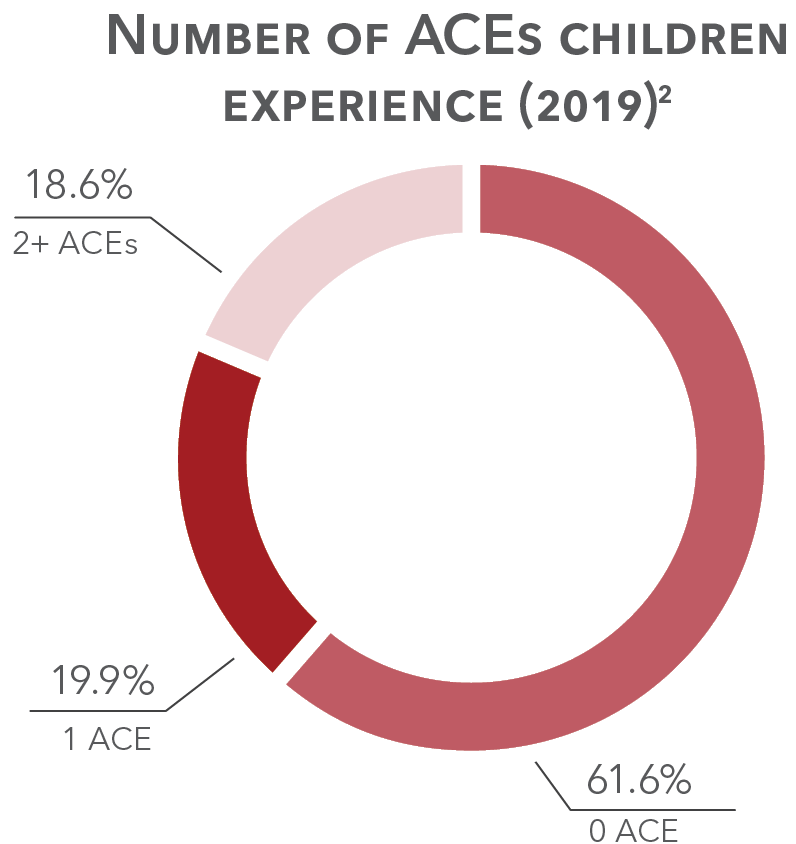
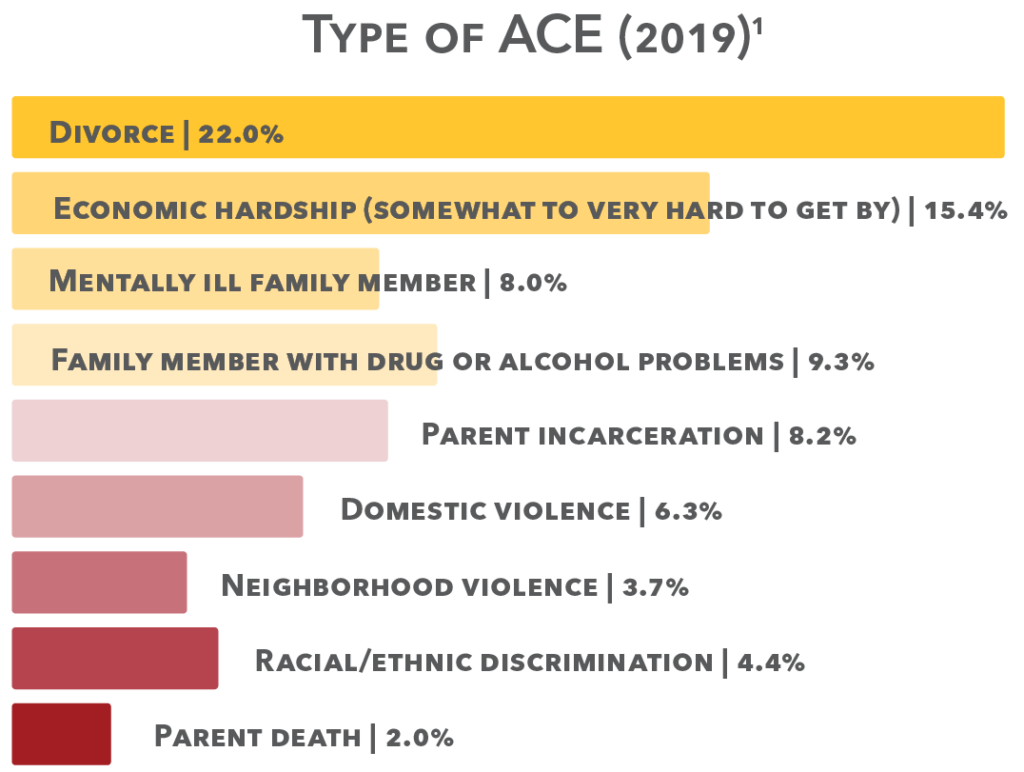
Adverse Childhood Experiences
Adverse childhood experiences (ACEs) are potentially traumatic events that can have negative, lasting effects on health and well-being. Experiencing multiple ACEs results in compounding effects, and there is growing evidence that it is the general experience of multiple ACEs, rather than the specific individual impact of any one experience that matters. The experience of ACEs extends beyond the child and can cause consequences for the whole family and community.
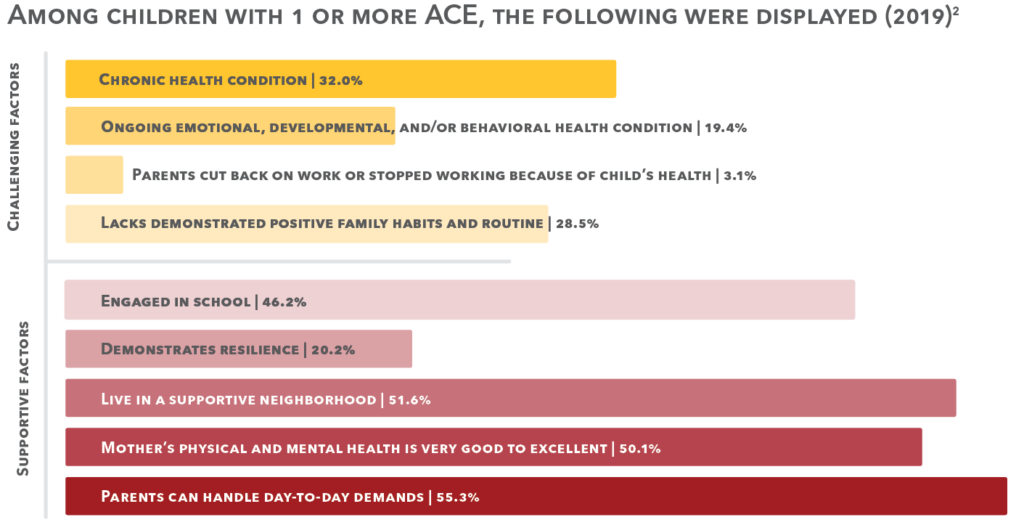
2. 2019 National Survey of Children’s Health.
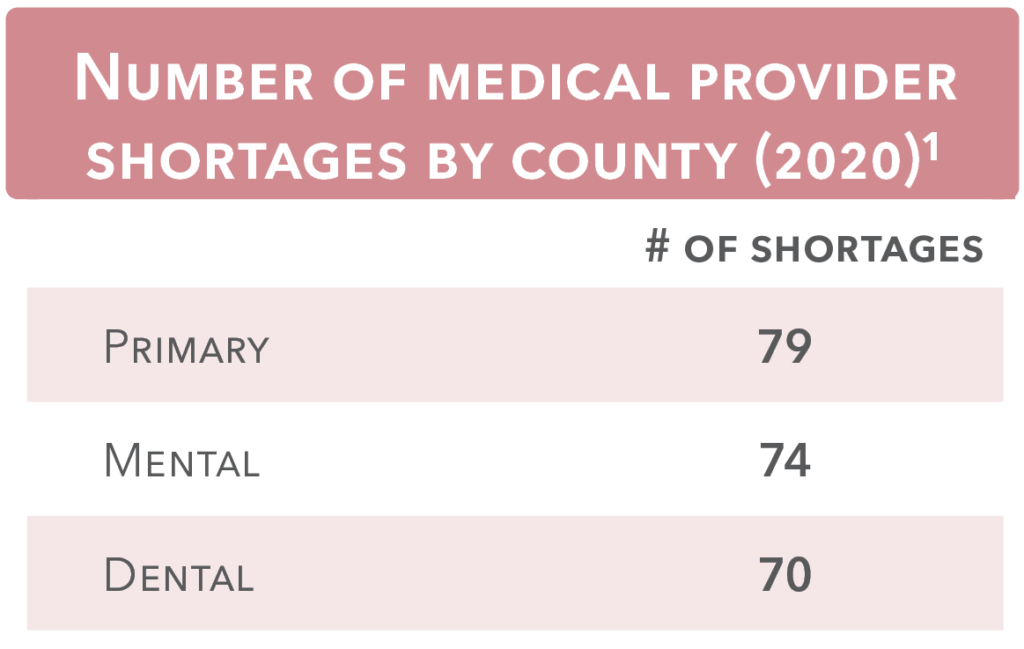
Health Services
Health professional shortage areas are designations that indicate a shortage of health care providers in the areas of primary care, mental health care, or dental health care. Shortages fall into three categories:¹
1. Geographic areas – a shortage of providers for the
entire population within an area
2. Population groups – a shortage of providers within
an area for a specific high need population
3. Facilities – health care facilities within an area have
a shortage of health professionals to meet their needs
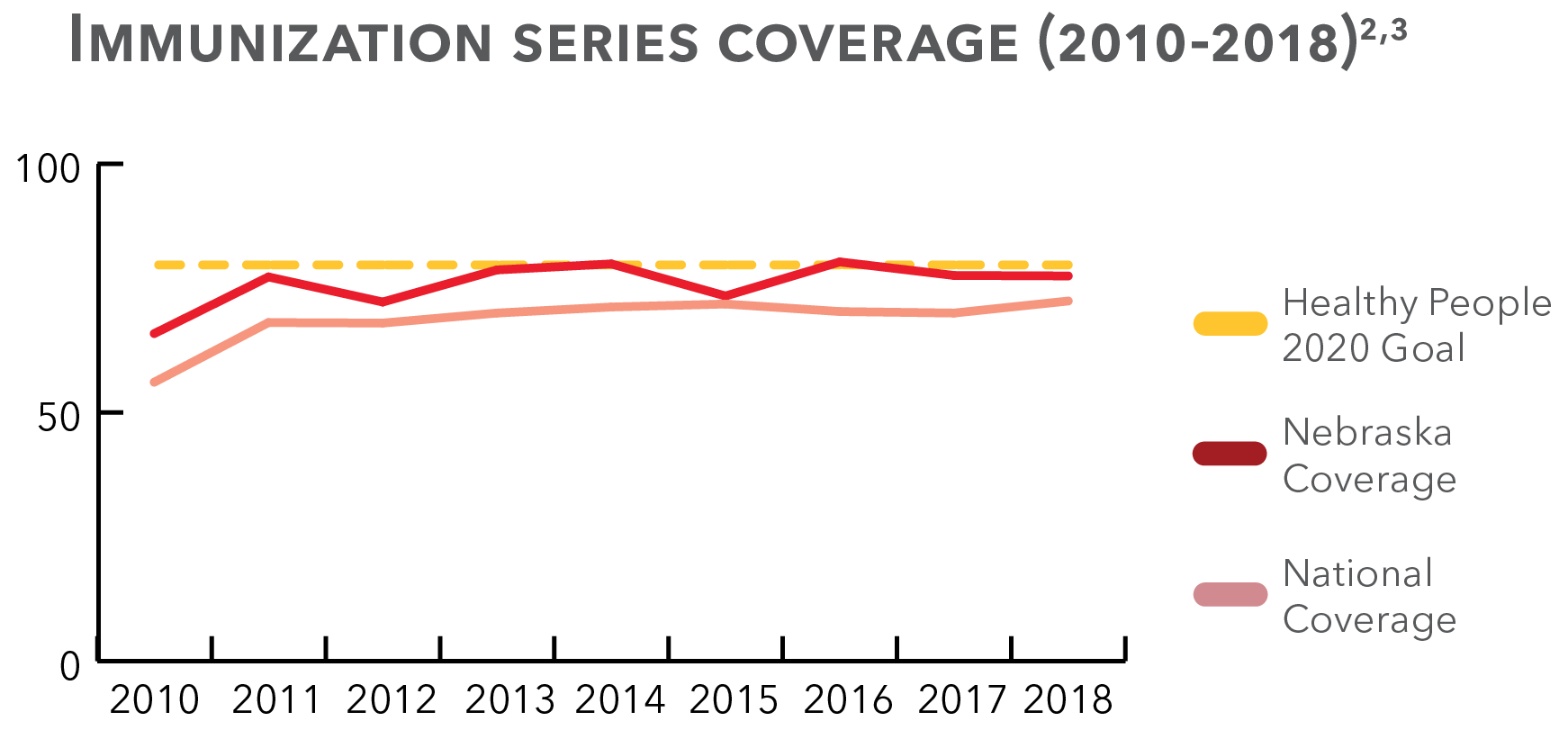
Immunizations (2018)2
77.8% of Nebraska children had received the primary immunization series* by age three.
84.0% of Nebraska teens were immunized against meningitis caused by types A, C, W, and Y.
66.6% of Nebraska teen girls and 59.0% of Nebraska teen boys completed their HPV vaccine series.
78.7% of children had a preventive medical visit in the past year.2
80.1% of children had a preventive dental visit in the past year.2
37.1% of children had one or more current health conditions.3
90.1% of children are in very good to excellent health.3
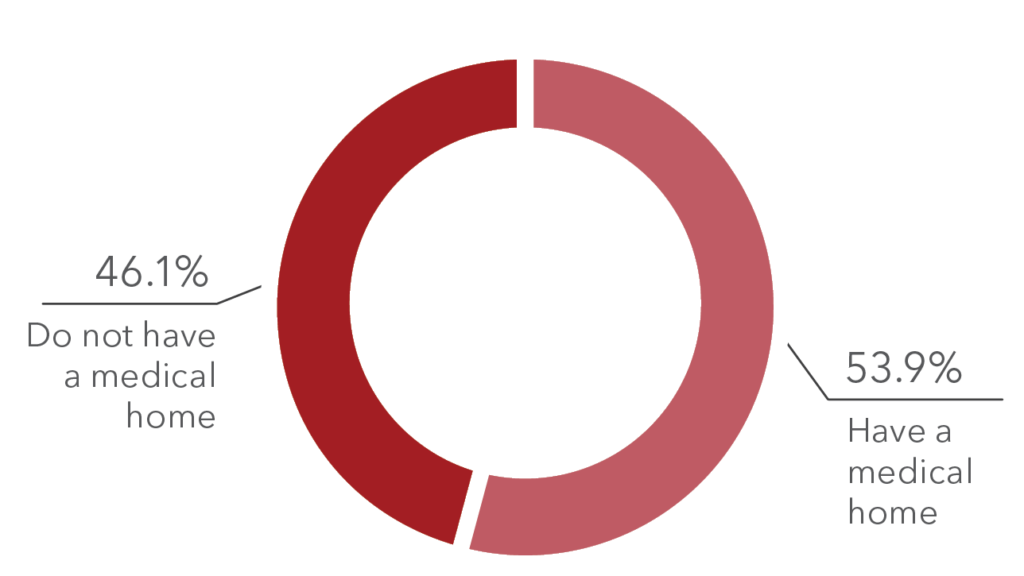
Children with a Medical home (2019)3,4
A patient-centered medical home is a primary care physician or provider that serves as a child’s usual source of care. It is an important mechanism for coordination of all segments of health – physical, behavioral, and oral.
2. National Immunization Survey-Child, 2018.
*Series 4:3:1:3:3:1:4
3. 2018-2019 National Survey of Children’s Health, National Performance Measure 11.
4. 2018-2019 National Survey of Children’s Health, National Performance Measure 13.2.
5. 2018 National Survey of Children’s Health, Health Care Access and Quality, Indicator 4.1a.